I’m writing this as both a registered nurse who works for an allergist, and also as a food allergy and EOE mom with over a decade of experience.
Nurses are caregivers, teachers, advocates, scientists, artists, healers and problem solvers. The ironic part is, so are food allergy moms!
Nurses, my Food Allergy Mamas need your help!
What’s the big deal, anyway?
The statistics recently changed and are impressive: 32 million Americans have food allergies, 1 in 13 children and 1 in 10 adults. An allergic reaction to food can quickly become life threatening.
When my daughter received this diagnosis, I was stunned. Not only did I have to re-learn how to feed her, I also had to learn how to keep her safe. I quickly realized this also impacted our entire family and how we lived everyday life.
I never expected this to happen to my child!
I was angry.
Why?
Like many of you amazing & highly skilled nurses, I never learned anything about food allergy management in my education or training.
I thought there was a lot of hype, and not many facts.
I was wrong!
Many health care professionals, including nurses, do not understand how to care for patients with food allergies or food allergic related conditions. This includes basic care needs like feeding, administering medications, and even using skin, hair, and hygiene products on such patients.
April 4, 2019, An 11 year old child with a milk allergy died from anaphylaxis after being given a whitening toothpaste by her dentist.
The toothpaste contained milk protein. Not one person noticed this critical ingredient- not the dentist, nor the parent or the child.
Quite frankly, I’m not sure I would have noticed it either. Milk in toothpaste? I will never forget this beautiful child or the difficult lessons we learned in the food allergy community after her death.
Toothpaste! This is how serious food allergies are, and it shows the constant vigilance that is required to stay safe.
I have worked on medical floors, procedural areas, intensive care units and the emergency room setting. Patient trays, turkey sandwiches, peanut butter and graham crackers would come and go. I never heard the words: Food Allergy.
I’m afraid to admit it, what if I did?
Would I have rolled my eyes and thought to myself, “This is not a hotel!”
My daughter and I were told that by a nurse, when my then 12 year old was hospitalized and kept in isolation with the flu.
I tried to explain to the nurse her food allergic related condition called, eosinophilic esophagitis. She never heard of it. Neither did I, until my child was diagnosed! This is why I share our story.
I do understand how a busy nurse might think such patients are being high maintenance, but they’re not.
To help my nursing colleagues, here are 5 ways to Take Better Care of Your Food Allergic Patients:
1. Believe them.

Photo by Pixabay on Pexels.com
If they land in your ER, please do not lecture or tell them they over reacted, or should have given an antihistamine first. This is a myth.
If they have given epinephrine, I will tell you from my first hand experience, they are truly shaken by this whole ordeal.
Tell them they did a good job!
They made the difficult decision to administer this life saving drug, call 911 and land in your care. They did their best to stop an anaphylactic reaction from potentially becoming fatal.
Our life saving mantra is: “Epi First, Epi Fast” if suspecting anaphylaxis!
Next, please monitor these patients. This is why we call 911 and go to the Emergency Room after administering epinephrine. It’s not because epinephrine is dangerous.
Allergic reactions can return! A second and more serious reaction, called a biphasic reaction, can happen up to 72 hours after the first! This is an important fact to know for discharge teaching.
2. Please to not eat in patient care areas.

Photo by Mehran B on Pexels.com
There’s nothing more unsettling than coming into the hospital or doctor’s office and seeing a jar of mixed nuts or treats open, on the desk.
We are not joking when it comes to something called cross contact. We know nurses need to eat on the go, and breaks are few and far between. But please, wash up after eating.
Like microbes, food proteins love to hang around on surfaces until thoroughly wiped away with a commercial cleaner.
Please wash your hands before examining us or touching our things. Remember, hand sanitizers do not remove food proteins, only soap and water or hand wipes do! Thank you!
3. Do not give your food allergic patient ANYTHING to eat or drink without asking first.

Photo by Leah Kelley on Pexels.com
Allergens love to hide in the most unsuspecting foods, like ice pops! Yes, even some ice pops contain common allergens or may be made on shared equipment with other allergens.
We are not rude or picky eaters. We have to read every label for possible allergens and may even have to contact companies to find out if their products are safe for us. This is a standard part of food allergy management.
We do appreciate any help we can get on this, especially with the hospital’s dietary department and kitchen.
Allergic Living Magazine did an excellent piece on this topic. It’s an eye opening read about being hospitalized with food allergies. Hospitals are realizing this is a patient safety issue. You can read it here.
4. Ask the Pharmacist if medications contain allergens.

Photo by Pixabay on Pexels.com
Allergens hide in the strangest places! They are found in medications, injectables, inhalers, eye drops, ointments, etc. These are technically called excipients.
Please double check with the pharmacy. Ask if any prescribed medications contain your patient’s allergens. We need your voice to help keep us safe.
5. Ask your patient if they have an Anaphylaxis Emergency Action Plan & a Board Certified Allergist.
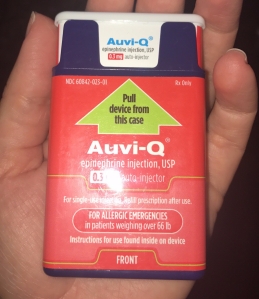
The Auvi Q, an epinephrine auto injector that talks you through how to use it, step by step!
An Anaphylaxis Emergency Action Plan is similar to what nurses commonly call a standing order. It is a document signed by the patient’s allergist.
An Anaphylaxis Emergency Action Plan tells the patient exactly what to do if they accidentally eat or bite into something containing their allergen, or are experiencing signs of anaphylaxis.
While discussing this topic, this is also an excellent time to review with your patient how to administer their epinephrine auto injector.
If your patient doesn’t have a board certified allergist managing their care, or if this is a new diagnosis, it’s time for a referral!
Food allergy management is a specialty area of medicine. A board certified allergist is the expert on this topic. Having an allergist can really help improve patient care and quality of life through ongoing education and support.
I hope these 5 tips help you provide the best care possible to your food allergic patients!
As we like to say in this food allergy life, “We’re not crazy. We’re Vigilant.”
If you come across a patient who could use some extra support, please send them to FAACT, The Food Allergy & Anaphylaxis Connection Team: www.foodallergyawareness.org
or to the support group I co-lead, Friends Helping Friends Food Allergy Support Group.

Great blog, Susan! I’ll never forget being at Boston Children’s Hospital about 12 years ago when Ella had to have a hernia operation, and they called from the recovery room to say that she was slowly waking up and they’d be giving her a popsicle to soothe her throat from the anesthesia – I asked about the ingredients – they thought I was crazy – and sure enough, the popsicle had CASEIN in it!! Yikes. A milk protein about to be given to a patient, post-surgery; it just goes to show that even in the best of the best hospitals, mistakes can happen and you can never stop being on top of things.
LikeLiked by 2 people
Thank you, Jesse! I appreciate you sharing your child’s experience. There is a tremendous gap in food allergy education among nurses because we simply did not see this volume of food allergic patients in the past!
Food allergies were rare, and maybe at most we would hear about shellfish allergies.
We need to close this gap because it is a patient safety issue.
Feeding a food allergic patient is just as serious as medication administration.
Lives are at risk, in the case of anaphylactic food allergies.
Who wants to put their patient into anaphylaxis because of an ice pop!?! Not me or any other nurse I know!
Yikes!!
I hope this blog helps make a dent! It’s a start, in any event.
LikeLike
This is important for dietitians and hospital dietary services, too. My son went into anaphylaxis when a meal tray was served to him that was not safe – even though dietary, nursing and his chart all documented the food allergy. The dietitian assured me the meals would be safe. The nurses thought I was over-reacting when I told them he was going to go into anaphylaxis as soon as I realized the meal tray error. All of them witnessed (in horror) anaphylaxis for the first time. Years later, I ran into one of the nurses in the hospital hallway. She said that she’d never forget us because of what she witnessed that day.
LikeLiked by 2 people
Thank you so much for sharing your very important experience, Lynda. I can see how this can easily happen in the busy hospital setting. There is a major gap in food allergy education. Our nurses are on the front line here & this education is critical! Thank you again!
LikeLike
Yes, this education and awareness is important, so thank you!! When my daughter was admitted to the hospital for anaphylaxis, we had to explain multiple times to the food service staff that she could not have any food in her room with nuts, and I had to explain the risk of cross-contamination. On top of that, in the patient kitchen/snack room on her floor, there were packages of peanut butter everywhere – which is the last thing you want to see when you are in the hospital with your child who almost died for ingesting that very thing. The nurses were amazing – it’s just an awareness/ education issue overall because when you are in that environment, you feel safe and trust what the caretakers are giving you, not realizing they may not be aware.
LikeLiked by 2 people
Yes to #2. The LAST thing you want to hear behind the ER curtain is that pizza was just delivered when you’re there with your child who is anaphylactic to milk protein. To follow that, they offered my child chocolate pudding 😬
LikeLiked by 1 person
With my son’s first anaphylaxis, the pediatric ER doctor went against my and our allergist’s orders to observe him for a longer time. He said “bi-phasic reactions don’t really happen.” Flash forward to one half hour later when I had to Epi him for the second time at home and by the time the paramedics fot there 3 minutes later his throat was closing. Nearly intubated during and ICU overnight stay.
His latest stay had me educating the resident on FPIES and why I had to Epi him because of it.
I have learned after his first stay that there is literally nothing safe he could eat in a hospital, including his elemental drink, so I keep an emergency food bag packed all the time with non perishables by an emergency overnight bag. They tried to send us safe food based on how s allergies (all listed for dietary) and received meals that were far from safe.
I have more but I’d like to finish with words of gratitude for everyone who does go out of their way for us at the hospital because they’ve seen him quite a bit now. The common theme with these professionals is that they all LISTENED. That’s what we need to convey.
LikeLiked by 2 people
Great job! Thank you! I would add: allow family to bring the patient safe food from home in the hospital. They freak out when you do that. I end up living on protein bars sneaked in. I don’t know what I’d do if I didn’t have a purse to hide them in. I simply can’t also have the stress of worrying about the food at the same time.
LikeLike
Absolutely! Us food allergy Moms typically carry a stash of safe snacks in our purse! I was thankful for family & friends who brought by daughter safe food to eat when she was hospitalized. Thanks for commenting! It’s always good to be prepared.
LikeLike
Amazing article Susan. Loved your comments on toothpastes with hidden allergens. “Recaldent” is an example of a dentally distributed product which contains milk protein. (See Recaldent FAQ section). If a toothpaste mentions calcium or phosphorus binding to enamel, go to website information on ingredients. Besides being an nurse and allergy advocate, I am also a registered dental hygienist. These products are great for tooth enamel IF you aren’t milk-protein sensitive.
LikeLike
This timely piece is well written and so important. Thank you Kelly !
LikeLike
Great information about food allergies ! Thanks for Sharing!
Keep posting… We are at Medical Tourism company in India. Click to know more http://www.healingtouristry.com
LikeLiked by 1 person
Thank you!
LikeLike